ERLEADA® (apalutamide), First-and-Only Next-Generation Androgen Receptor Inhibitor with Once-Daily, Single-Tablet Option Offers Prescribers More Flexibility to Treat Patients
Prostate cancer is one of the most common cancers in the U.S., with 288,300 new cases estimated to be diagnosed in 2023.1 Many prostate cancer patients will present with comorbidities, including diabetes, depression, urinary issues, sexual dysfunction and cardiovascular diseases, all of which follow specific therapeutic regimens.2 Prostate cancer treatment depends on several factors, including the stage of cancer, possible side effects, and a patient’s personal preferences and overall health.3
It is common for patients to be taking medications for both their comorbid conditions and their prostate cancer, which can quickly add up to 10-12 different medications per day.4 All of a patient’s varied medication protocols and number of pills can be burdensome to manage. According to recent research reported in CURE Today, roughly 20% to 30% of prostate cancer patients reported difficulty with swallowing oral medications as prescribed.5 Clinicians must consider many aspects of the patient and his disease in setting a course of therapy and care.
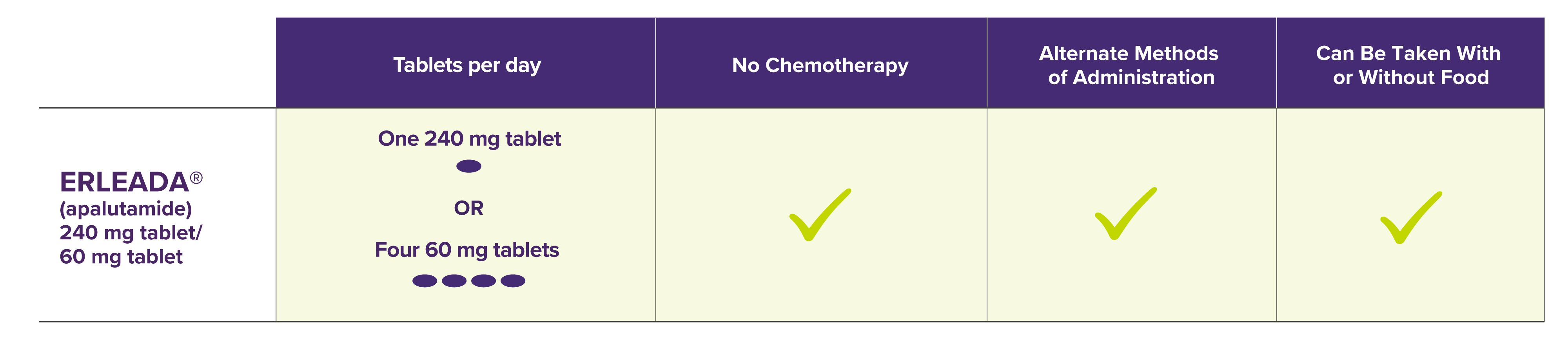
For patients with non-metastatic castration-resistant prostate cancer (nmCRPC) or metastatic castration-sensitive prostate cancer (mCSPC), ERLEADA® (apalutamide) may be a convenient and flexible treatment option. ERLEADA® is the first-and-only novel androgen receptor inhibitor (ARI) with a new once-daily, 240 mg single-tablet option (the 60 mg tablets remain available for patients who prefer to take four tablets once-daily). ERLEADA® is also the only ARI with labeling to include approved alternate methods of administration for patients who have difficulty swallowing tablets whole. The 60 mg tablets continue to have an approved option for dispersing with applesauce, while the 240 mg tablet is approved for dispersing in orange juice, noncarbonated water or applesauce. The 240 mg tablet may also be administered through a feeding tube. For detailed instructions on administration, please see the full Prescribing Information for ERLEADA®.
“ERLEADA® has a well-established clinical profile, having treated more than 30,000 patients in the U.S. and having demonstrated significant improvement in overall survival for both nmCRPC and mCSPC,” said Luca Dezzani, M.D., U.S. Vice President, Medical Affairs, Solid Tumor, Janssen Scientific Affairs, LLC. “We understand that each patient’s needs are unique. With the addition of a once-daily, single-tablet option of ERLEADA® and several alternate methods of administration, we hope to provide a therapy choice that is flexible and convenient.”
Both approved indications for ERLEADA® were based on two Phase 3 randomized, double-blind, placebo-controlled clinical studies, which evaluated ERLEADA® combined with androgen deprivation therapy (ADT) compared with a placebo plus ADT. In 1,207 patients with nmCRPC, the SPARTAN clinical trial demonstrated treatment with ERLEADA® plus ADT significantly improved median metastasis-free survival (MFS) compared with placebo plus ADT. The median MFS for the ERLEADA® plus ADT arm was 40.5 months (3.4 years) vs. 16.2 months (1.4 years) for the placebo plus ADT arm, representing an improvement of MFS by 2 years (24.3 months). Treatment with ERLEADA® plus ADT significantly decreased the risk of distant metastasis or death by 72% compared with placebo plus ADT (HR=0.28; 95% CI: 0.23, 0.35; P<0.0001).6,7
In 1,052 patients with mCSPC, the prespecified final analysis of the TITAN clinical trial demonstrated treatment with ERLEADA® plus ADT reduced the risk of death by 35% vs. placebo plus ADT (median overall survival [OS] was not estimable [NE] vs. 52.2 months; HR=0.65; 95% CI: 0.53, 0.79; median follow-up time was 44.0 months). At 48 months the survival rate was 65.1% in the ERLEADA® plus ADT arm and 51.8% in the placebo plus ADT arm. The primary analysis of TITAN data showed treatment with ERLEADA® plus ADT reduced the risk of death by 33% compared with placebo plus ADT (HR=0.67; 95% CI: 0.51, 0.89; P=0.0053; median follow-up time was 22.7 months). Median OS was not estimable in either arm at the median follow-up of 22.7 months.8,9
More information on the SPARTAN and TITAN trials including study design, patient characteristics, safety, and efficacy results is available at https://www.erleadahcp.com/efficacy
Both 240 mg and 60 mg ERLEADA® tablet strengths are available by prescription through existing specialty pharmacy networks.
ABOUT ERLEADA®
INDICATIONS
ERLEADA® (apalutamide) is an androgen receptor inhibitor indicated for the treatment of patients with:
- Metastatic castration-sensitive prostate cancer (mCSPC)
- Non-metastatic castration-resistant prostate cancer (nmCRPC)
IMPORTANT SAFETY INFORMATION FOR ERLEADA®
WARNINGS AND PRECAUTIONS
Cerebrovascular and Ischemic Cardiovascular Events— In a randomized study (SPARTAN) of patients with nmCRPC, ischemic cardiovascular events occurred in 3.7% of patients treated with ERLEADA® and 2% of patients treated with placebo. In a randomized study (TITAN) in patients with mCSPC, ischemic cardiovascular events occurred in 4.4% of patients treated with ERLEADA® and 1.5% of patients treated with placebo. Across the SPARTAN and TITAN studies, 4 patients (0.3%) treated with ERLEADA® and 2 patients (0.2%) treated with placebo died from an ischemic cardiovascular event. Patients with history of unstable angina, myocardial infarction, congestive heart failure, stroke, or transient ischemic attack within 6 months of randomization were excluded from the SPARTAN and TITAN studies.
In the SPARTAN study, cerebrovascular events occurred in 2.5% of patients treated with ERLEADA® and 1% of patients treated with placebo. In the TITAN study, cerebrovascular events occurred in 1.9% of patients treated with ERLEADA® and 2.1% of patients treated with placebo. Across the SPARTAN and TITAN studies, 3 patients (0.2%) treated with ERLEADA®, and 2 patients (0.2%) treated with placebo died from a cerebrovascular event.
Cerebrovascular and ischemic cardiovascular events, including events leading to death, occurred in patients receiving ERLEADA®. Monitor for signs and symptoms of ischemic heart disease and cerebrovascular disorders. Optimize management of cardiovascular risk factors, such as hypertension, diabetes, or dyslipidemia. Consider discontinuation of ERLEADA® for Grade 3 and 4 events.
Fractures— In a randomized study (SPARTAN) of patients with nmCRPC, fractures occurred in 12% of patients treated with ERLEADA® and in 7% of patients treated with placebo. In a randomized study (TITAN) of patients with mCSPC, fractures occurred in 9% of patients treated with ERLEADA® and in 6% of patients treated with placebo. Evaluate patients for fracture risk. Monitor and manage patients at risk for fractures according to established treatment guidelines and consider use of bone-targeted agents.
Falls — In a randomized study (SPARTAN), falls occurred in 16% of patients treated with ERLEADA® compared with 9% of patients treated with placebo. Falls were not associated with loss of consciousness or seizure. Falls occurred in patients receiving ERLEADA® with increased frequency in the elderly. Evaluate patients for fall risk.
Seizure —In two randomized studies (SPARTAN and TITAN), 5 patients (0.4%) treated with ERLEADA® and 1 patient treated with placebo (0.1%) experienced a seizure. Permanently discontinue ERLEADA® in patients who develop a seizure during treatment. It is unknown whether anti-epileptic medications will prevent seizures with ERLEADA®. Advise patients of the risk of developing a seizure while receiving ERLEADA® and of engaging in any activity where sudden loss of consciousness could cause harm to themselves or others.
Severe Cutaneous Adverse Reactions— Fatal and life-threatening cases of severe cutaneous adverse reactions (SCARs), including Stevens‑Johnson syndrome/toxic epidermal necrolysis (SJS/TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS) occurred in patients receiving ERLEADA®.
Monitor patients for the development of SCARs. Advise patients of the signs and symptoms of SCARs (eg, a prodrome of fever, flu-like symptoms, mucosal lesions, progressive skin rash, or lymphadenopathy). If a SCAR is suspected, interrupt ERLEADA® until the etiology of the reaction has been determined. Consultation with a dermatologist is recommended. If a SCAR is confirmed, or for other Grade 4 skin reactions, permanently discontinue ERLEADA®[see Dosage and Administration (2.2)].
Embryo-Fetal Toxicity— The safety and efficacy of ERLEADA® have not been established in females. Based on findings from animals and its mechanism of action, ERLEADA® can cause fetal harm and loss of pregnancy when administered to a pregnant female. Advise males with female partners of reproductive potential to use effective contraception during treatment and for 3 months after the last dose of ERLEADA®[see Use in Specific Populations (8.1, 8.3)].
ADVERSE REACTIONS
The most common adverse reactions (≥10%) that occurred more frequently in the ERLEADA®-treated patients (≥2% over placebo) from the randomized placebo-controlled clinical trials (TITAN and SPARTAN) were fatigue, arthralgia, rash, decreased appetite, fall, weight decreased, hypertension, hot flush, diarrhea, and fracture.
Laboratory Abnormalities — All Grades (Grade 3-4)
- Hematology — In the TITAN study: white blood cell decreased ERLEADA® 27% (0.4%), placebo 19% (0.6%). In the SPARTAN study: anemia ERLEADA® 70% (0.4%), placebo 64% (0.5%); leukopenia ERLEADA® 47% (0.3%), placebo 29% (0%); lymphopenia ERLEADA® 41% (1.8%), placebo 21% (1.6%)
- Chemistry — In the TITAN study: hypertriglyceridemia ERLEADA® 17% (2.5%), placebo 12% (2.3%). In the SPARTAN study: hypercholesterolemia ERLEADA® 76% (0.1%), placebo 46% (0%); hyperglycemia ERLEADA® 70% (2%), placebo 59% (1.0%); hypertriglyceridemia ERLEADA® 67% (1.6%), placebo 49% (0.8%); hyperkalemia ERLEADA® 32% (1.9%), placebo 22% (0.5%)
Rash —In 2 randomized studies (SPARTAN and TITAN), rash was most commonly described as macular or maculopapular. Adverse reactions of rash were 26% with ERLEADA® vs 8% with placebo. Grade 3 rashes (defined as covering >30% body surface area [BSA]) were reported with ERLEADA® treatment (6%) vs placebo (0.5%).
The onset of rash occurred at a median of 83 days. Rash resolved in 78% of patients within a median of 78 days from onset of rash. Rash was commonly managed with oral antihistamines, topical corticosteroids, and 19% of patients received systemic corticosteroids. Dose reduction or dose interruption occurred in 14% and 28% of patients, respectively. Of the patients who had dose interruption, 59% experienced recurrence of rash upon reintroduction of ERLEADA®.
Hypothyroidism — In 2 randomized studies (SPARTAN and TITAN), hypothyroidismwas reported for 8% of patients treated with ERLEADA® and 1.5% of patients treated with placebo based on assessments of thyroid-stimulating hormone (TSH) every 4 months. Elevated TSH occurred in 25% of patients treated with ERLEADA® and 7% of patients treated with placebo. The median onset was at the first scheduled assessment. There were no Grade 3 or 4 adverse reactions. Thyroid replacement therapy, when clinically indicated, should be initiated or dose adjusted.
DRUG INTERACTIONS
Effect of Other Drugs on ERLEADA® — Co-administration of a strong CYP2C8 or CYP3A4 inhibitor is predicted to increase the steady-state exposure of the active moieties. No initial dose adjustment is necessary; however, reduce the ERLEADA® dose based on tolerability [see Dosage and Administration (2.2)].
Effect of ERLEADA® on Other Drugs
CYP3A4, CYP2C9, CYP2C19, and UGT Substrates — ERLEADA® is a strong inducer of CYP3A4 and CYP2C19, and a weak inducer of CYP2C9 in humans. Concomitant use of ERLEADA® with medications that are primarily metabolized by CYP3A4, CYP2C19, or CYP2C9 can result in lower exposure to these medications. Substitution for these medications is recommended when possible or evaluate for loss of activity if medication is continued. Concomitant administration of ERLEADA® with medications that are substrates of UDP-glucuronosyl transferase (UGT) can result in decreased exposure. Use caution if substrates of UGT must be co-administered with ERLEADA® and evaluate for loss of activity.
P-gp, BCRP, or OATP1B1 Substrates— Apalutamide is a weak inducer of
P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), and organic anion transporting polypeptide 1B1 (OATP1B1) clinically. Concomitant use of ERLEADA® with medications that are substrates of P-gp, BCRP, or OATP1B1 can result in lower exposure of these medications. Use caution if substrates of P-gp, BCRP, or OATP1B1 must be co-administered with ERLEADA® and evaluate for loss of activity if medication is continued.
Please see the full Prescribing Information for ERLEADA®.
This article is sponsored by Janssen Biotech, Inc.
###
____________________
1 American Cancer Society. Cancer Facts & Figures 2023. Accessed May 11, 2023.
https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2023/2023-cancer-facts-and-figures.pdf
2 Li H, Hodgson E, Watson L, Shukla A, Nelson JJ. Comorbidities and concomitant medication use in men with prostate cancer or high levels of PSA compared to matched controls: A GPRD analysis. J Cancer Epidemiol. 2012;2012:1-13. doi:10.1155/2012/291704
3 Prostate cancer – types of treatment. Published February 10, 2023. Accessed March 29, 2023. https://www.cancer.net/cancer-types/prostate-cancer/types-treatment
4 Given BA, Given CW, Sikorskii A, Vachon E, Banik A. Medication burden of treatment using oral cancer medications. Asia-Pacific J Oncol Nurs. 2017;4(4):275-282. doi:10.4103/apjon.apjon_7_17
5 Benyon B. Easy-to-swallow drug shows similar results to Zytiga in patients with metastatic prostate cancer. Cure Today. Published January 9, 2023. Accessed March 29, 2023. https://www.curetoday.com/view/easy-to-swallow-drug-shows-similar-results-to-zytiga-in-patients-with-metastatic-prostate-cancer
6 ERLEADA® [Prescribing Information]. Horsham, PA: Janssen Biotech, Inc.
7 Smith MR, Saad F, Chowdhury S, et al. N Engl J Med. 2018;378(15):1408-1418.
8 Chi KN, Chowdhury S, Chung BH, et al. J Clin Oncol. 2021;39(20):2294-2303.
9 Chi KN, Agarwal N, Bjartell A, et al. N Engl J Med. 2019 Jul 4;381(1)13-24.
