The Queensland General Practice Liaison Network is a multidisciplinary collaboration of clinicians working to improve the patient journey between general practice and hospitals.
The network supports the work of General Practice Liaison Officers and provides expert direction and advice relating to communication, clinical handover, and collaboration across primary and secondary care.
Queensland has 16 Hospital and Health Services (HHSs) and seven Primary Health Networks (PHNs). Most of these employ General Practice Liaison Officers (GPLOs).
Queensland’s GPLOs play a unique role in identifying and addressing service gaps, facilitating appropriate clinical pathways, and improving transfer of care processes.
This includes providing direction and advice on communication, clinical handover, provider collaboration, supporting health system improvement, and promoting associated education and research.
The Queensland General Practice Liaison (QGPL) Network membership reflects various disciplines (GPs, nurses, allied health and administrative), geographical areas, and organisations involved in general practice liaison services in Queensland.
Member GPLOs are employed by different organisations, such as HHSs or PHNs; however, the network is funded by the Healthcare Improvement Unit, Clinical Excellence Queensland, Queensland Health and supported by PHNs.
Communication between GPLOs and general practice teams happens on many levels, including via individual, practice visits, email and social media, education events, newsletters, as well as interorganisational governance bodies, steering committees and/or executive meetings.
History
The QGPL Network was established in 2008 by General Practice Queensland. In 2012, Queensland Health funded 20 GPLO positions in the largest public hospitals under a state election commitment.
The role and function of the GPLO positions were based on recommendations described in the General Practice Queensland position paper: Enhancing integration: the General Practice Liaison Model, 2011.
From 2013, Queensland Health provided funding to CheckUP Australia (formerly General Practice Queensland) to partner and facilitate the QGPL Network.
Since May 2019, Country to Coast QLD (previously known as Central Queensland, Wide Bay, Sunshine Coast PHN) has partnered with Queensland Health to coordinate the QGPL Network.
| Objectives of QGPL Network
Build the capacity and capability of GPLOs through the sharing of learning, experiences, resources and innovations Identify and share effective local strategies, solutions, and service delivery models to support wider implementation Reduce duplication of effort and promote effective and equitable use of resources and equity of access for patients Provide opportunities for network members to build mutually supportive and collaborative relationships Showcase achievements of the network and its members at local and state-wide levels Implement the QGPL Network work plan |
The work of GPLOs
The work of GPLOs can be varied, with some GPLOs involved in specific projects or programs and others working at a broad or strategic level.
GPLOs develop strong working relationships and partnerships across the health system to support collaborative models of care that promote care in the most appropriate settings, optimising resource use and minimising low value care.
Another common denominator is the focus on transfer of care and (electronic) communication between primary and secondary care.
GPLOs are in regular contact with clinicians across different environments who provide feedback.
This helps identify gaps and assists to solve practical problems (eg, communication breakdowns).
By working with non-clinical hospital and PHN staff, Queensland Health and community stakeholders (project teams, managers, executives), GPLOs contribute to interconnectedness of the health system and quality improvement.
A common scenario is that GPLOs receive feedback from GPs about the timeliness or quality of clinical handover from one or more hospital departments to general practice.
This can usually be resolved on an individual basis to ensure safe continuity of care of a particular patient, but may also result in a quality improvement initiative, such as within a department or hospital.
For example, in the Sunshine Coast, this mechanism has led to the introduction of a same-day discharge summary policy across all public hospitals.
Queensland GPLOs have been pivotal in progressing major initiatives, including GP Smart Referrals and other electronic communication tools, GP access to the Health Provider Portal, HealthPathways and new models of care such as hospital GPs with special interest (GPSIs). GPLOs provide clinical handover workshops for junior hospital doctors and help organise interprofessional education opportunities.
GPLOs are often members of hospital committees tasked with quality improvement or (clinical) governance related to transfer of care, communicating for safety or collaborative care initiatives.
For example, there is extensive representation from GPLOs on the statewide GP Smart Referrals and HealthPathways committees. In some areas GPLOs are managing the hospital GPSI program.
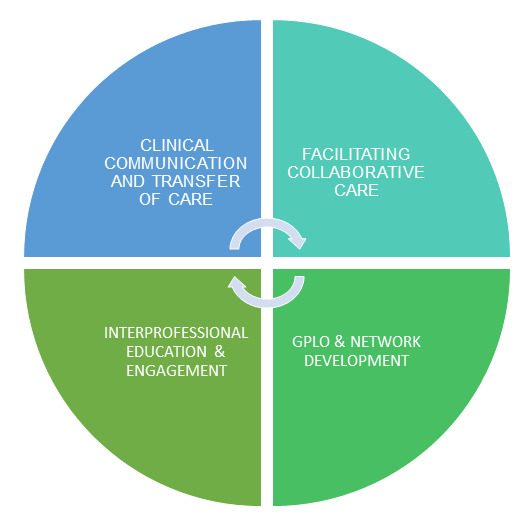
| GPLO focus on connecting care
Optimising the interface between general practice and hospital care is vital to improve patient experience, with enhancements focusing on: · Transfer of care Interprofessional education and engagement about integration mechanisms and associated models of care |
Below are some recent examples of projects Queensland GPLOs have been working on. For more information see the Queensland General Practice Liaison Network 2020–2022 Biennial report.
Shared COVID-19 response
During the coronavirus disease 2019 (COVID-19) pandemic, GPLOs, the QGPL Network and the Queensland HealthPathways Coordinators developed a suite of evidence-based clinical tools and communication mechanisms to support GPs, HHS and PHNs.
A shared response with all stakeholders enabled the delivery of coordinated, timely COVID-19 care in Queensland.
Virtual GP education
The COVID-19 pandemic has not only created challenges in health care delivery but has also disrupted in-person medical education events.
Supported by GPLOs, Children’s Health Queensland (CHQ) initiated the virtual knowledge sharing model Project ECHO, consolidated a relationship with the Royal Australian College of General Practitioners (RACGP), and built on the success of the annual Paediatric Masterclass for General Practice by delivering the RACGP’s webinar series.
GPLOs were involved in the organisation and coordination as well as presentation of the events.
GP Advice Program
The GP Advice Program aims to deliver strengthened relationships between specialists and GPs by providing GPs access to specialist advice to support patient care in the community and reducing low value face-to-face hospital care as well as waiting times.
The program was the result of feedback from GPs to GPLOs. GPLOs provided input in the design, workflow, key performance indicators and technical solutions.
With funding from the Department of Health, a proof-of-concept operational model was successful in delivering benefits for patients, GPs, specialists, and the health service.
The model will be implemented across other HHSs in Queensland.
Developing health assessments for children in out-of-home care
Across Queensland, there are over 12 000 children currently under a Child Protection Order.
Children’s Health Queensland report that many children in out-of-home care have undiagnosed disabilities and mental health concerns, are at higher risk of exposure to trauma, neglect and abuse and have poorer health than their peers.
GPLOs, GPs and Children’s Health Queensland jointly developed and implemented standardised health assessment templates for this group.
The templates can be uploaded into general practice software.
GPs with special interest
Lead by GPLOs, the GPSI program has been successfully implemented in the Sunshine Coast Hospital and Health Service and other areas of Queensland since 2018, and continues to expand with support from Clinical Excellence Queensland.
One of the main benefits is increased collaboration and understanding between GPs and hospital specialty teams.
The program is well received by GPs, hospital clinicians and patients.
The hospital GPSI model as an integrated workforce solution provides efficiency benefits for the health system across primary and secondary/tertiary care and high satisfaction levels for patients and clinicians.
Many of these benefits can only be achieved because hospital GPSIs continue their work as community GPs.
Conclusion
The work GPLOs do is person-centric and improves individual patient care and surrounding systems.
Due to the high degree of complexity of Australian health care, GPLOs succeed best where there are collaborative partnerships between general practice, HHSs and PHNs.
The support from Queensland Health, especially the Healthcare Improvement Unit, as well as PHNs, means the QGPL Network can continue to facilitate initiatives and grow the work GPLOs do to better connect our health care system.
Dr Edwin Kruys is a GP and General Practice Liaison Officer (GPLO) in the Sunshine Coast and Co-Chair of the Queensland General Practice Liaison (QGPL) Network.
Dr Toni Weller is a GP and GPLO in Townsville and Co-Chair of the QGPL Network.
Joanne Sweetser is a Principal Project Officer from the Healthcare Improvement Unit, Clinical Excellence Queensland, and a registered Occupational Therapist.
Karen Mansley is the Coordinator of the QGPL Network, Country to Coast QLD.
The statements or opinions expressed in this article reflect the views of the authors and do not necessarily represent the official policy of the AMA, the MJA or InSight+ unless so stated.
Subscribe to the free InSight+ weekly newsletter here. It is available to all readers, not just registered medical practitioners.
If you would like to submit an article for consideration, send a Word version to [email protected].
